Reimagining India’s family planning ecosystem: WOHLA’s market development partnerships approach
In India, the awareness and use of an expanded range of contraceptives, particularly hormonal options, have largely remained confined to the health sector. Historically, family planning has been narrowly viewed as a health intervention aimed at maternal health, with limited integration into broader social, economic, and community contexts. This health-centric focus has restricted awareness to traditional methods like sterilization, IUDs, and condoms, while overlooking modern contraceptive options, such as hormonal contraceptives, that address a wider range of reproductive health needs. Furthermore, socio-cultural taboos and minimal cross-sector collaboration have hampered efforts to normalize hormonal contraceptives. Important sectors like private healthcare, Common Service Centers (CSCs), businesses, and NGOs focused on women’s livelihoods have not been effectively engaged, limiting the reach and impact of family planning initiatives. Navigating this space therefore requires not only a comprehensive understanding of the larger environment in which contraceptives access is situated but also an ability to see the interconnectedness between various actors.
This is what the USAID/FHM Engage supported Women’s Health and Livelihood Alliance (WOHLA) is striving to do through its ecosystem approach to bolster the supply and demand of contraceptives and sexual and reproductive health (SRH) products, services, and information to women in underserved communities. WOHLA is targeting all the key market actors in the contraceptives value chain space and their interlinkages through its six-partnerships approach. The synergistic aim of these six partnerships is to improve and expand women’s knowledge of and access to a wide range of contraceptives to help meet their individual SRH needs. Let us take a closer look at how WOHLA is engaging with key stakeholders and deploying its six partnerships to create an enabling environment for the production, distribution, and consumption of contraceptive services and products in India.
1. Fostering new partnerships for manufacturers
Manufacturers face several challenges in expanding access to contraceptives, particularly due to regulatory inconsistencies. A key issue is the lack of harmonization in scheduling: while second-generation oral contraceptive pills (OCPs) are available over-the-counter in the public sector, commercial sector OCPs are restricted to prescription-only due to their Schedule H classification. This inconsistency hampers large-scale promotion and limits product availability. Additionally, manufacturers are seeking sustainable alternatives beyond social marketing companies, which primarily focus on subsidized, price-controlled second-generation OCPs. This limits the diversity of available contraceptive products. High costs associated with inefficient, outdated supply and demand management systems further complicate efforts to scale up production and distribution.
To overcome these barriers, manufacturers are increasingly turning to digital platforms for supply chain management and market expansion. Many have expressed interest in collaborating with FHM Engage to launch innovative OCPs tailored to women’s evolving reproductive needs. A significant component of this collaboration will be working with local partner, Access Health, in advocating for streamlined product scheduling, labeling, and championing the inclusion of new-generation contraceptives in Government of India-endorsed guidelines. These regulatory advancements would enable greater access to modern contraceptives, benefiting a broader population. A key objective is to facilitate partnerships with new supply chain and demand mobilization actors, enhancing private sector investment in both emergency contraceptive (EC) and oral contraceptive (OC) markets.
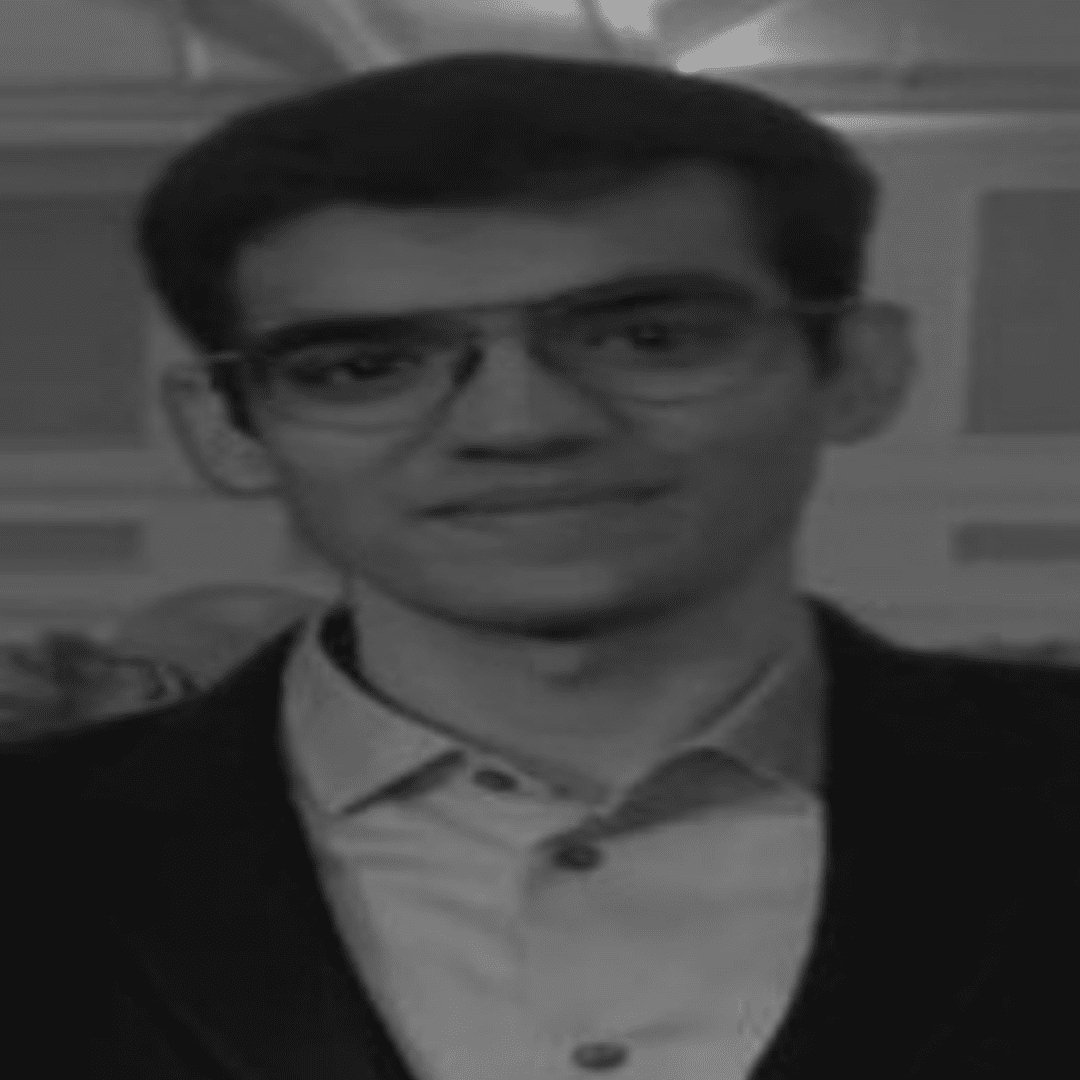
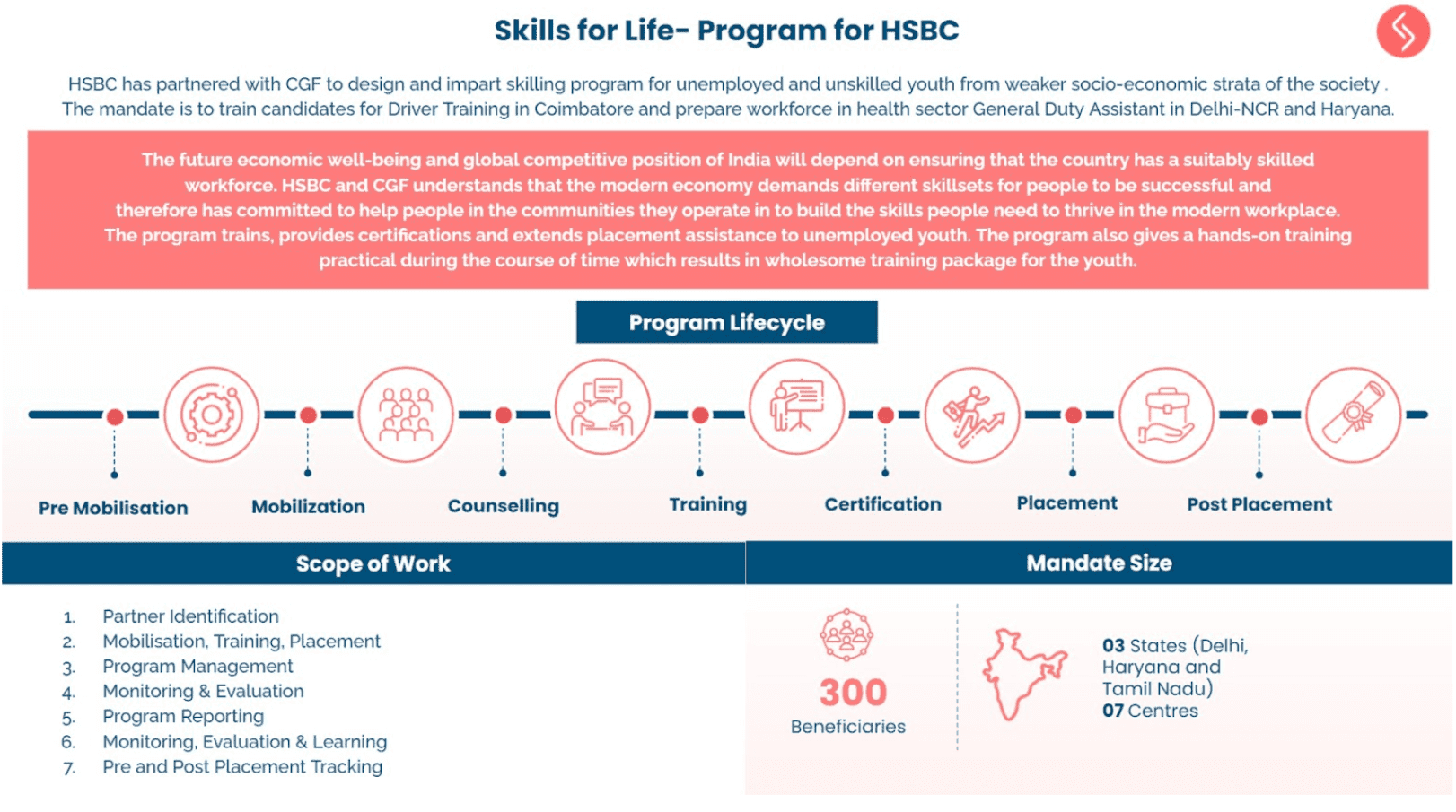
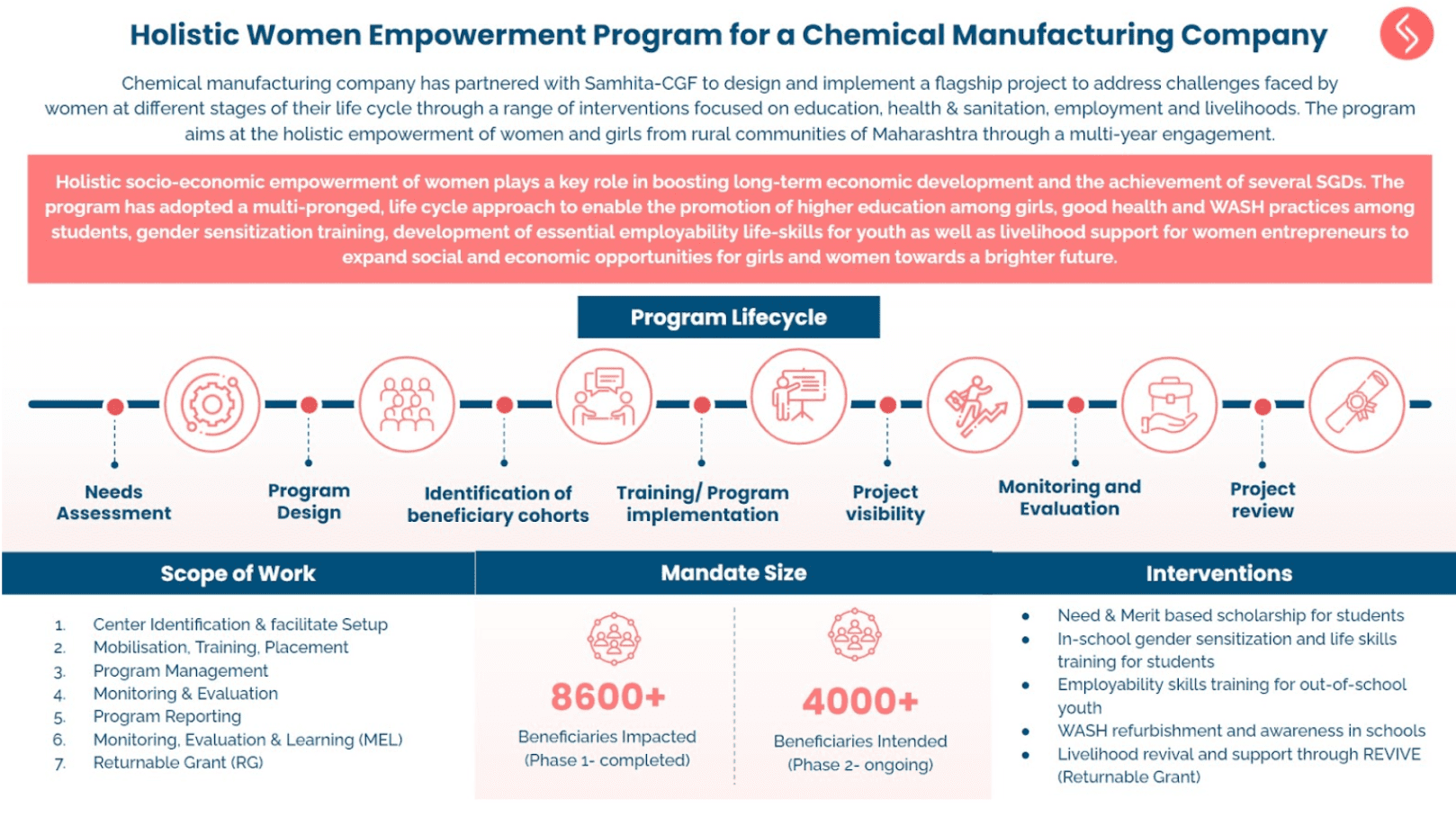
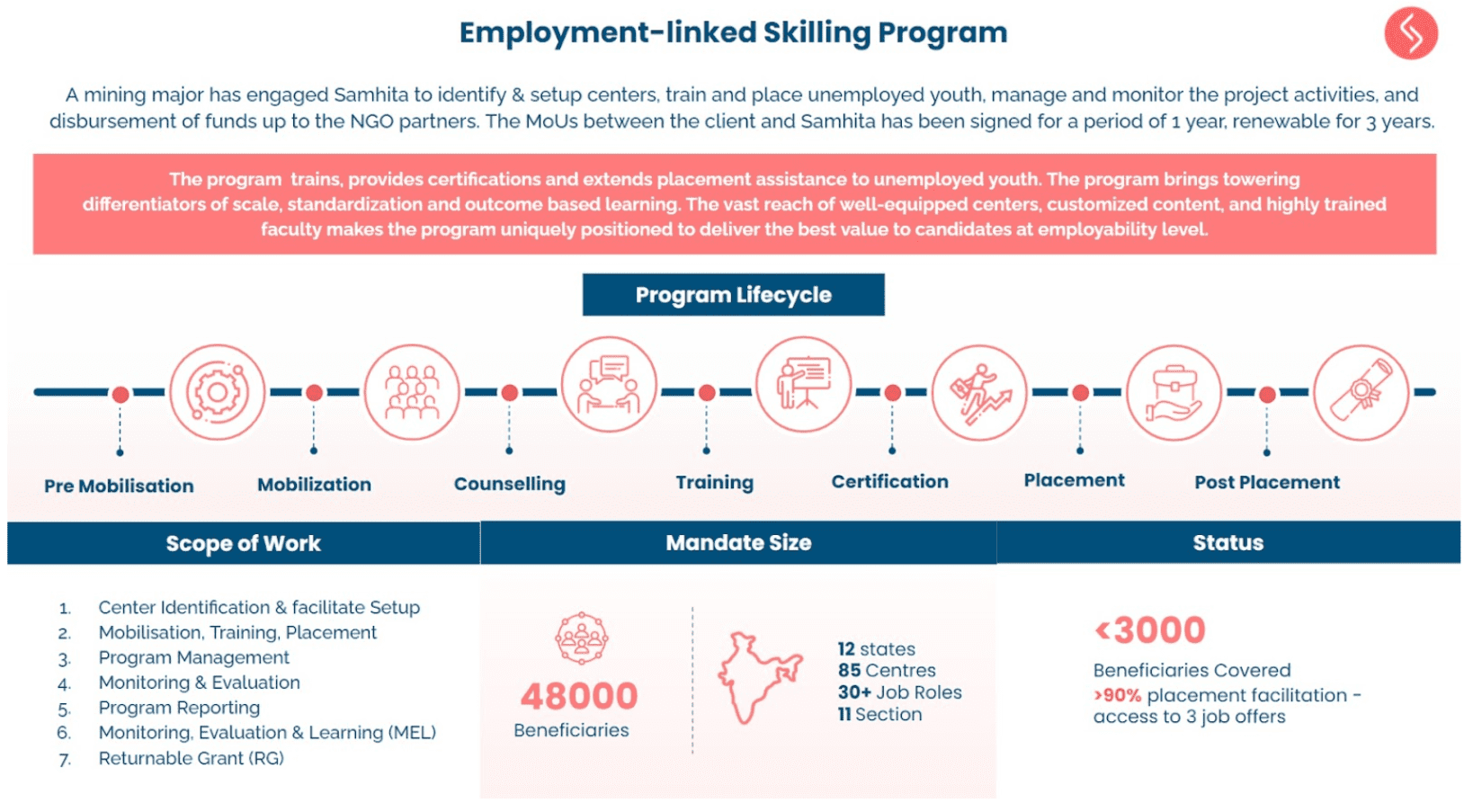
To support this initiative, WOHLA through co-founding partner, CGF-Samhita, is organizing regular discussions across product segments and regions to incentivize local manufacturers. The goal is to help manufacturers recognize their critical role in women’s empowerment and to encourage them to promote and market new brands and next-generation family planning and sexual/reproductive health products. This approach will not only diversify the market but also advance women’s health and economic empowerment.
2. Facilitating financing for distributors
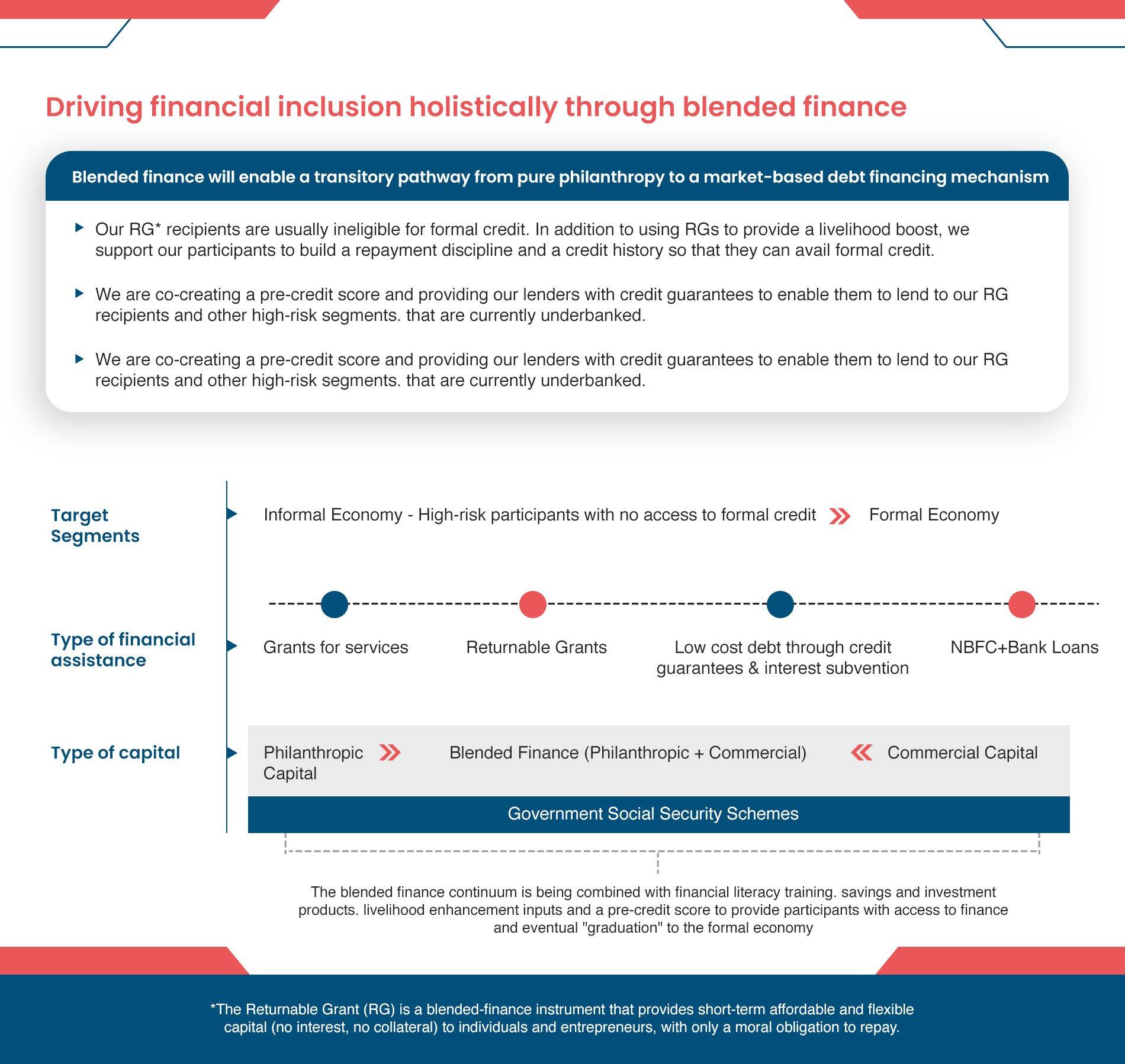
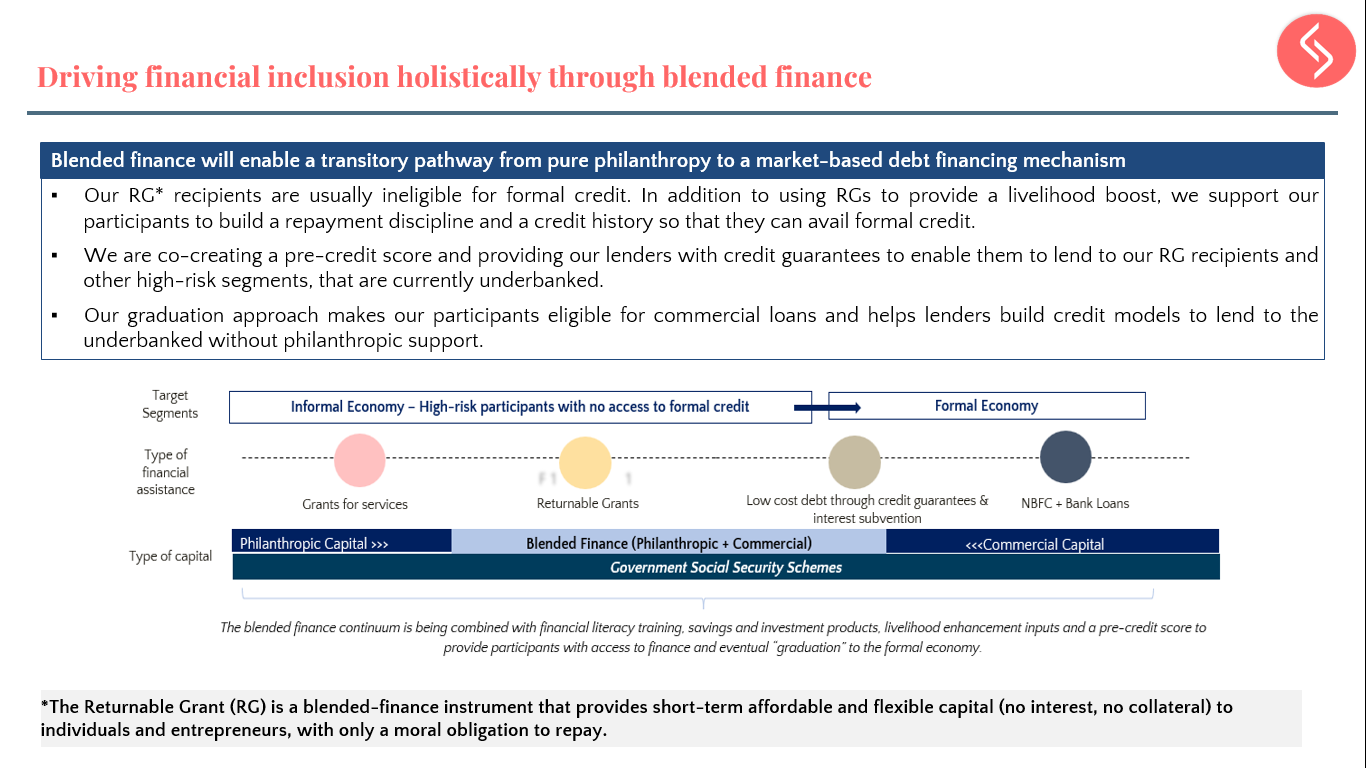
Distributors of family planning (FP) products play a crucial role as intermediaries between manufacturers and service providers, but they face significant challenges due to limited access to affordable financing. This financial strain hinders their ability to cover promotional expenses, particularly in smaller markets where manufacturers provide minimal marketing support. As a result, contraceptive options have reduced visibility and availability, impacting family planning access in underserved areas. To address this, WOHLA is working with distributors in key states—Delhi, Maharashtra, Karnataka, Meghalaya, and Assam—seeking to secure affordable financing to promote and upgrade their inventories, including newer FP/SRH products. By collaborating with government supported financial inclusion initiatives and banking and financing intermediaries like Appreciate, WOHLA aims to bridge the funding gap through working capital loans tailored for contraceptive inventory expansion. These loans will enable distributors to manage their stock without straining their finances. Additionally, WOHLA is exploring partnerships with distributor aggregators to pool demands of smaller distributors, enabling access to larger funding opportunities and better commercial terms. This approach helps distributors secure credit for both inventory and promotional expenses, ultimately expanding access to modern contraceptives in underserved communities.
3. Leveraging digital health channels and market intelligence
WOHLA’s third partnerships approach focuses on leveraging digital technology and market intelligence to enhance the demand for and supply of family planning (FP) products. To achieve this, WOHLHA is partnering with Pharmarack and Nivi to connect last-mile solution providers with consumers, using digital platforms to optimize FP access.
Pharmarack, India’s largest integrated B2B healthcare platform, combines technology, analytics, logistics, and financing, reaching over 10,000 distributors and 150,000 retailers nationwide. Under FHM Engage, Pharmarack’s platform has been customized to track trade in contraceptive products between distributors and chemists. By gathering data on sales volume, stock levels, and pricing, this system provides valuable insights into high-demand areas, distribution gaps, and trends in contraceptive uptake. This market intelligence is shared with manufacturers and distributors to ensure they align their strategies with consumer needs, improving supply chain efficiency and product availability.
WOHLA’s approach also addresses the growing need for manufacturers to adopt a hybrid model—combining physical and digital channels to connect effectively with last-mile providers. By using geo-tagged referrals and a chatbot linked to local doctors and pharmacies, WOHLA ensures users are directed to trusted healthcare providers, reducing distribution costs and enhancing the reach of sexual and reproductive health (SRH) products. Nivi, a digital health company, complements this strategy with its AI-powered chatbot (askNivi), providing consumers with anonymous, interactive FP guidance. Nivi onboards private service providers and pharmacies, enabling users to scan QR codes in local establishments to access personalized FP messages and referrals. Nivi’s online marketing through platforms like Facebook and YouTube further strengthens connections between providers and consumers, ensuring FP products and services reach youth and underserved communities effectively.
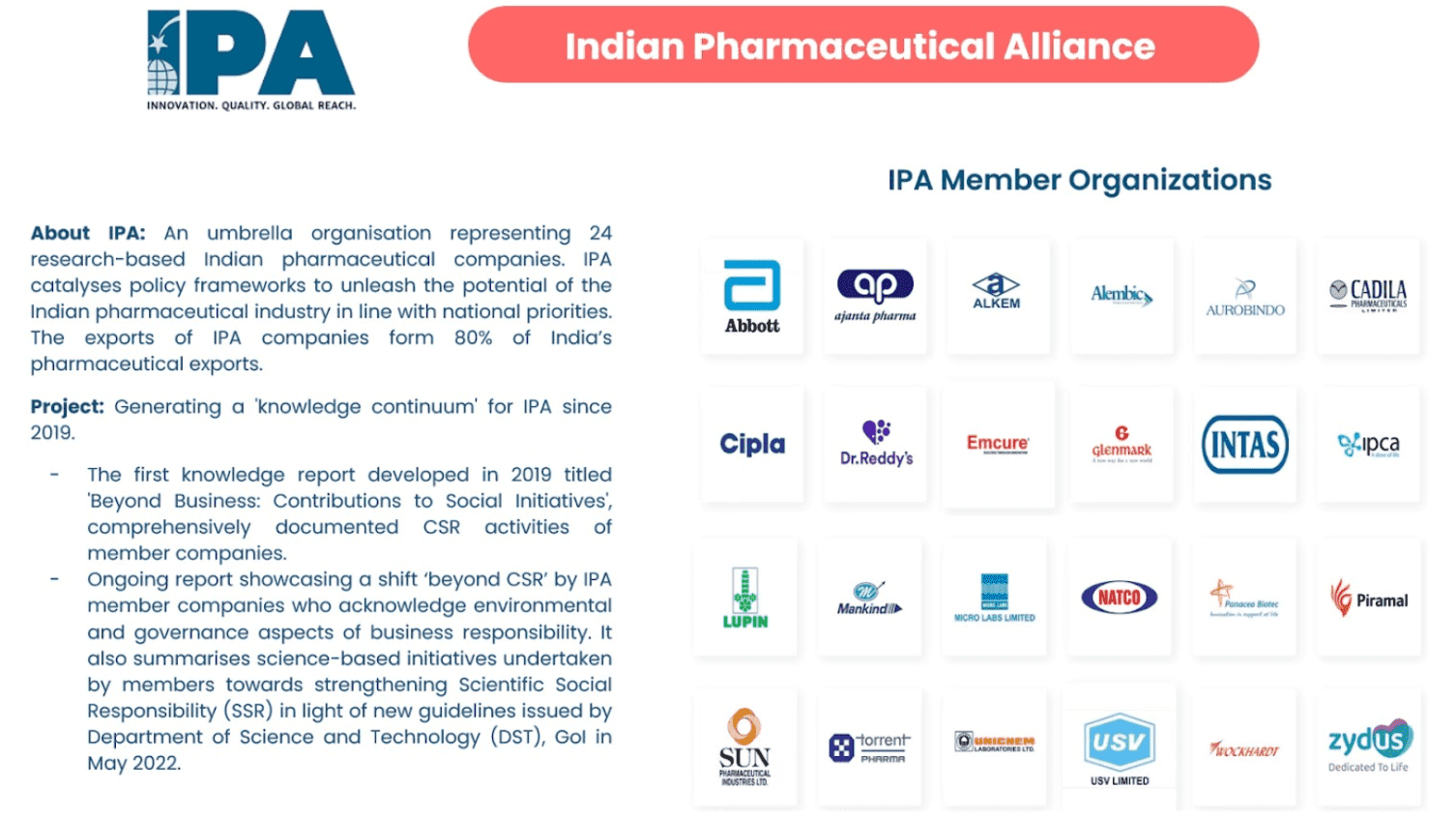
4. Promoting women’s health and economic security
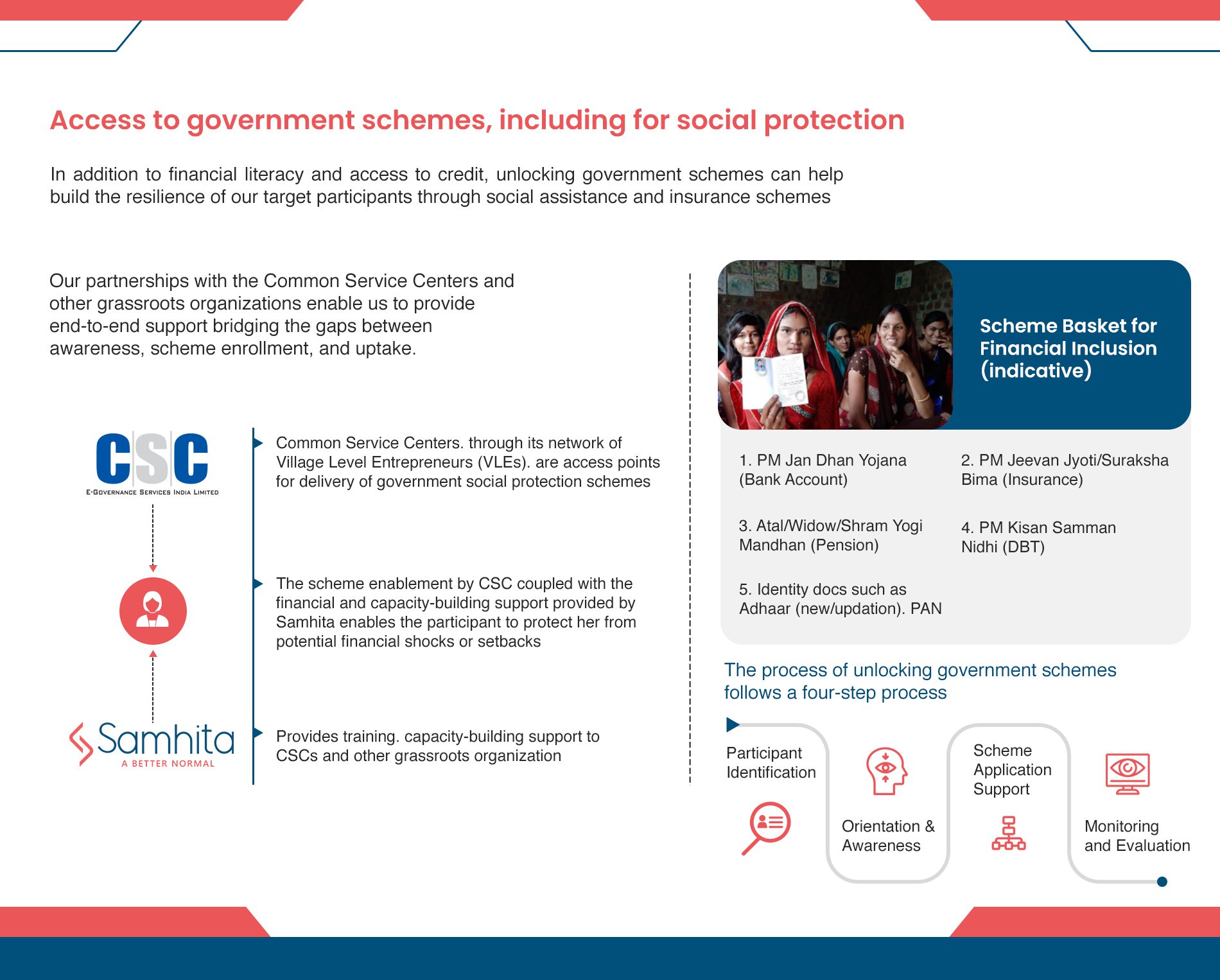
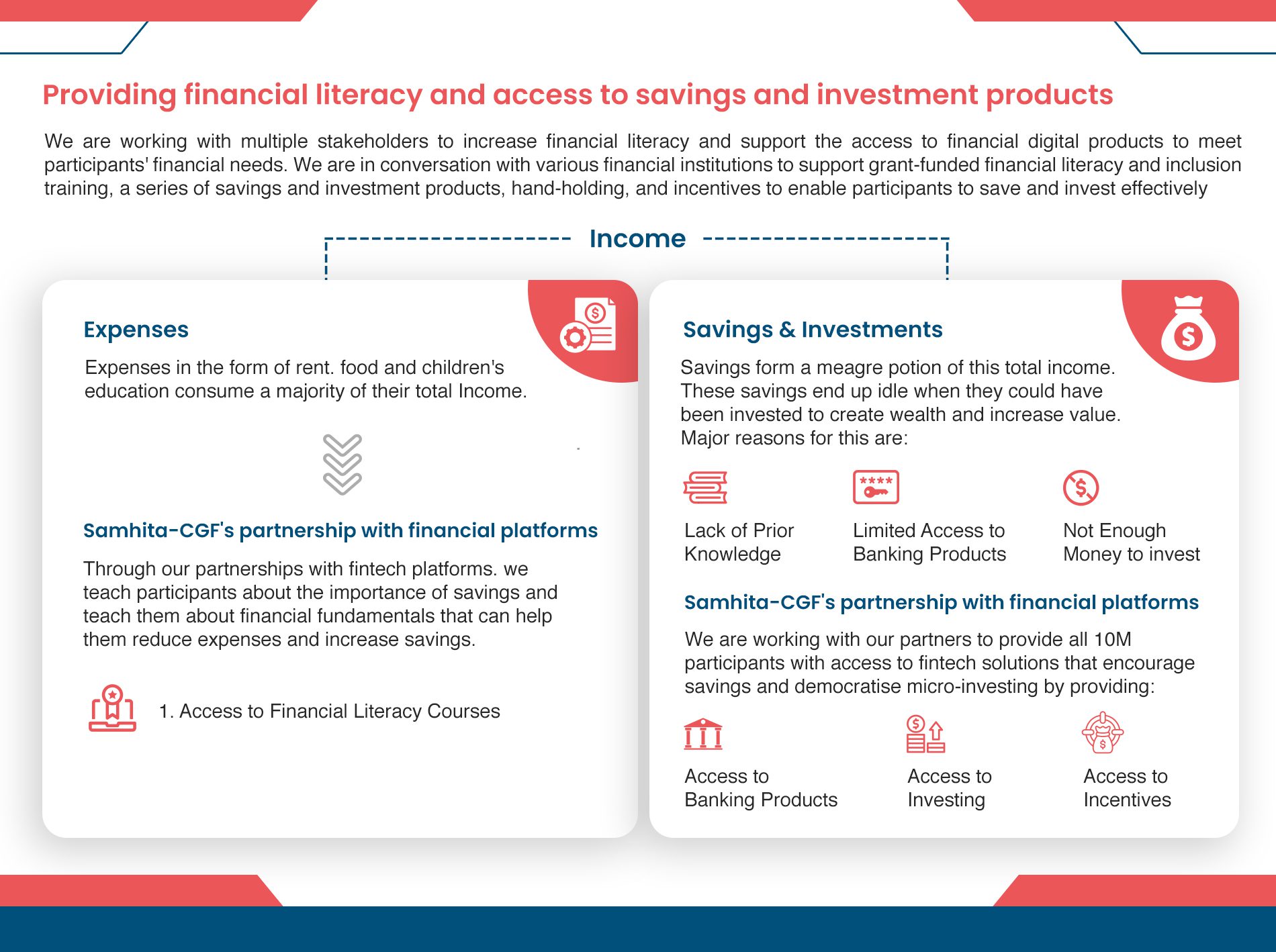
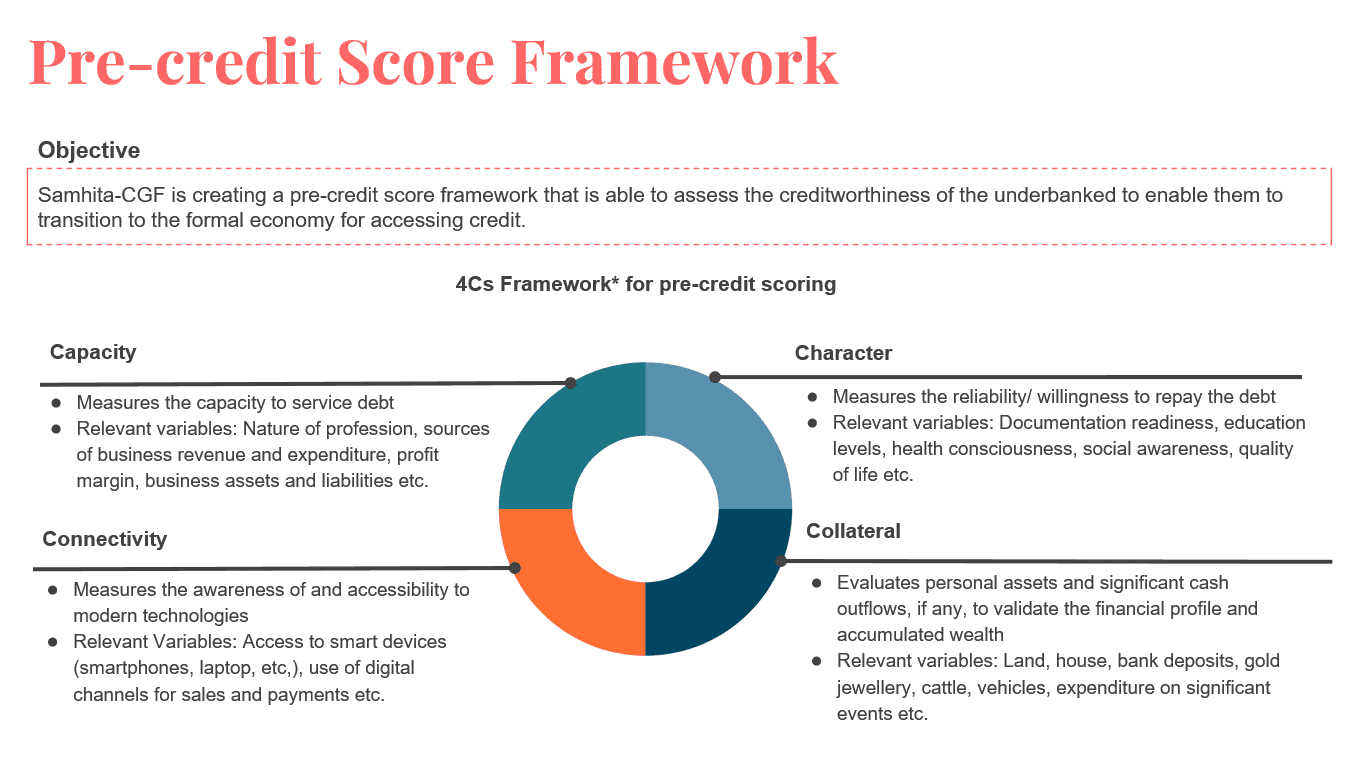
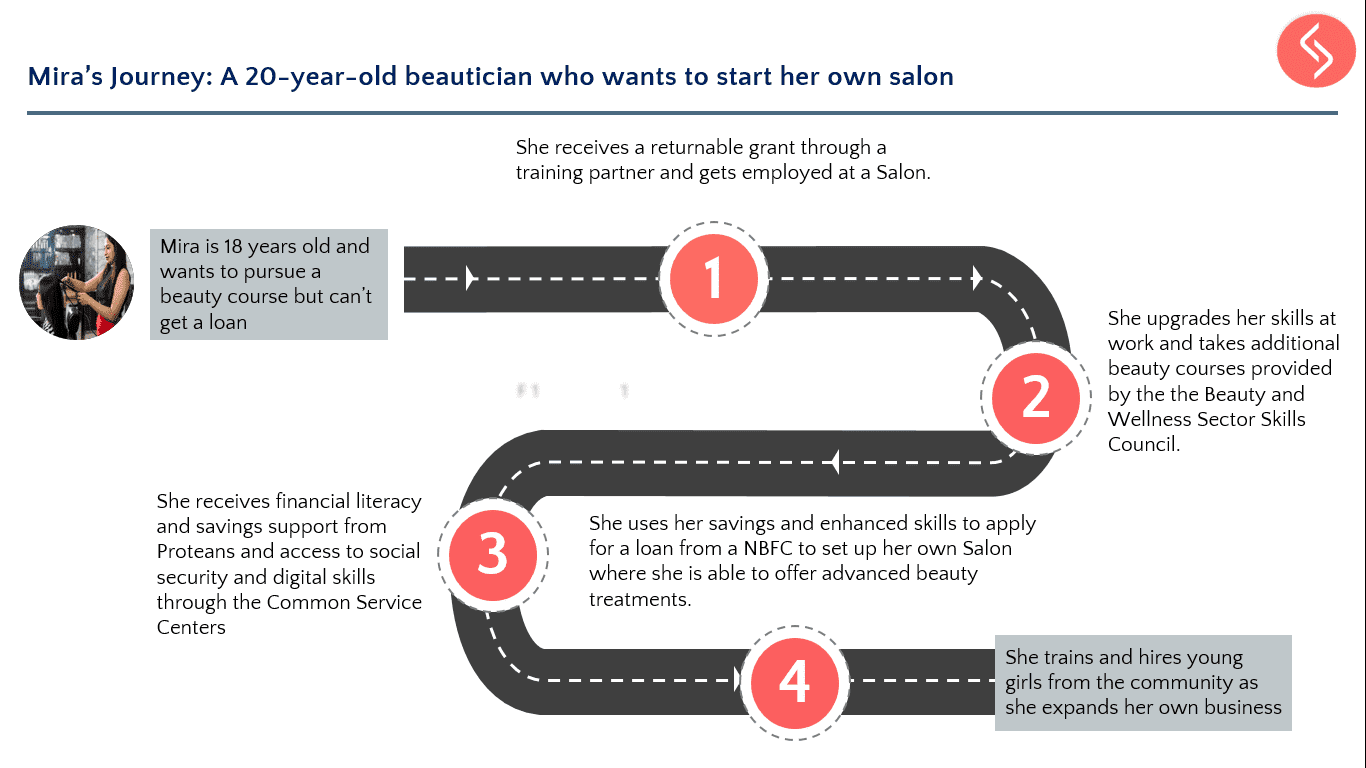
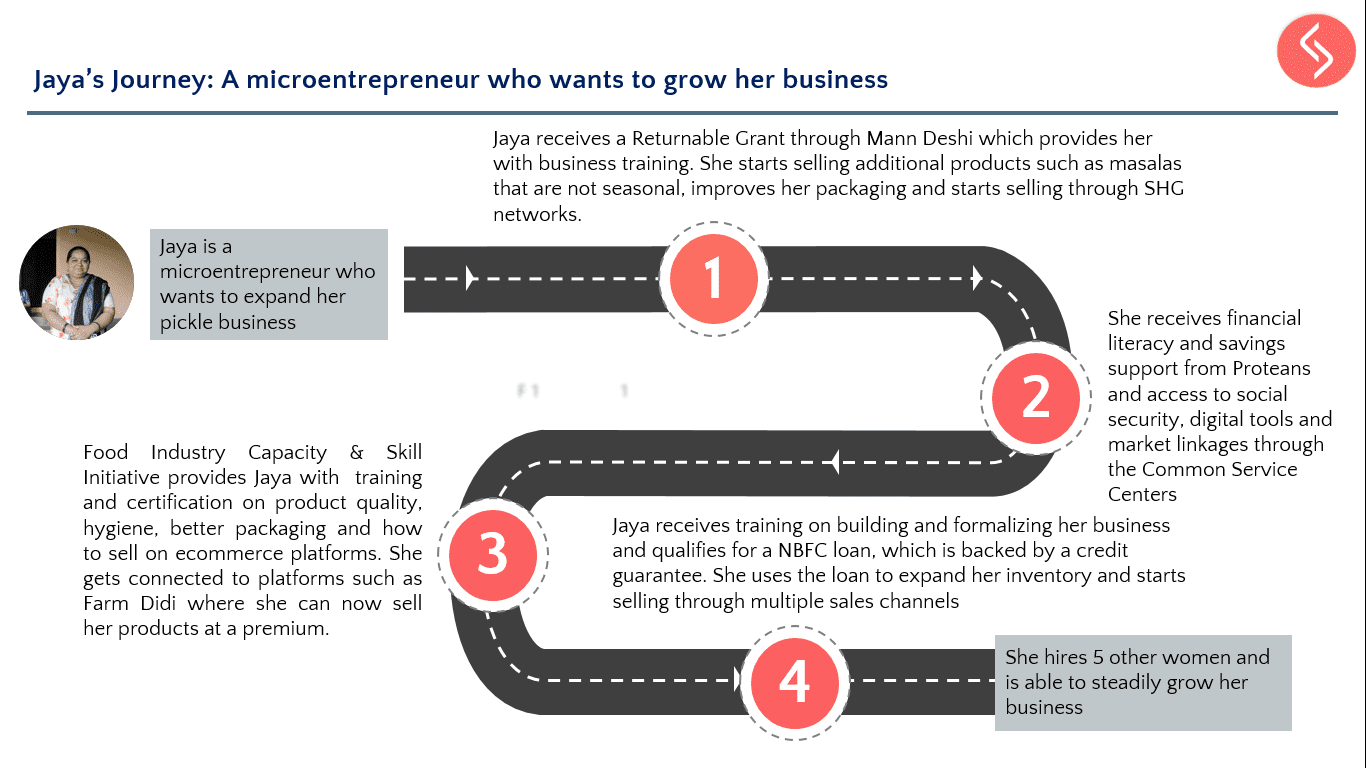
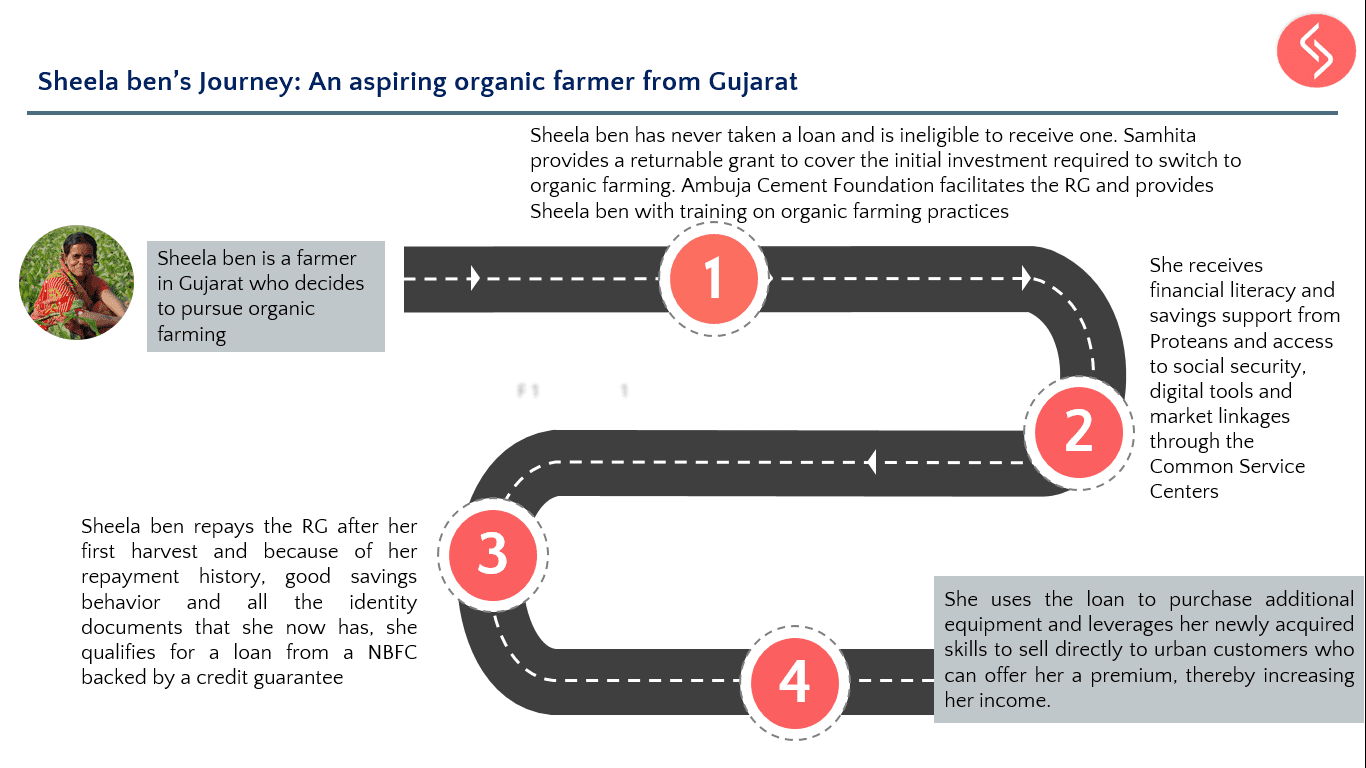
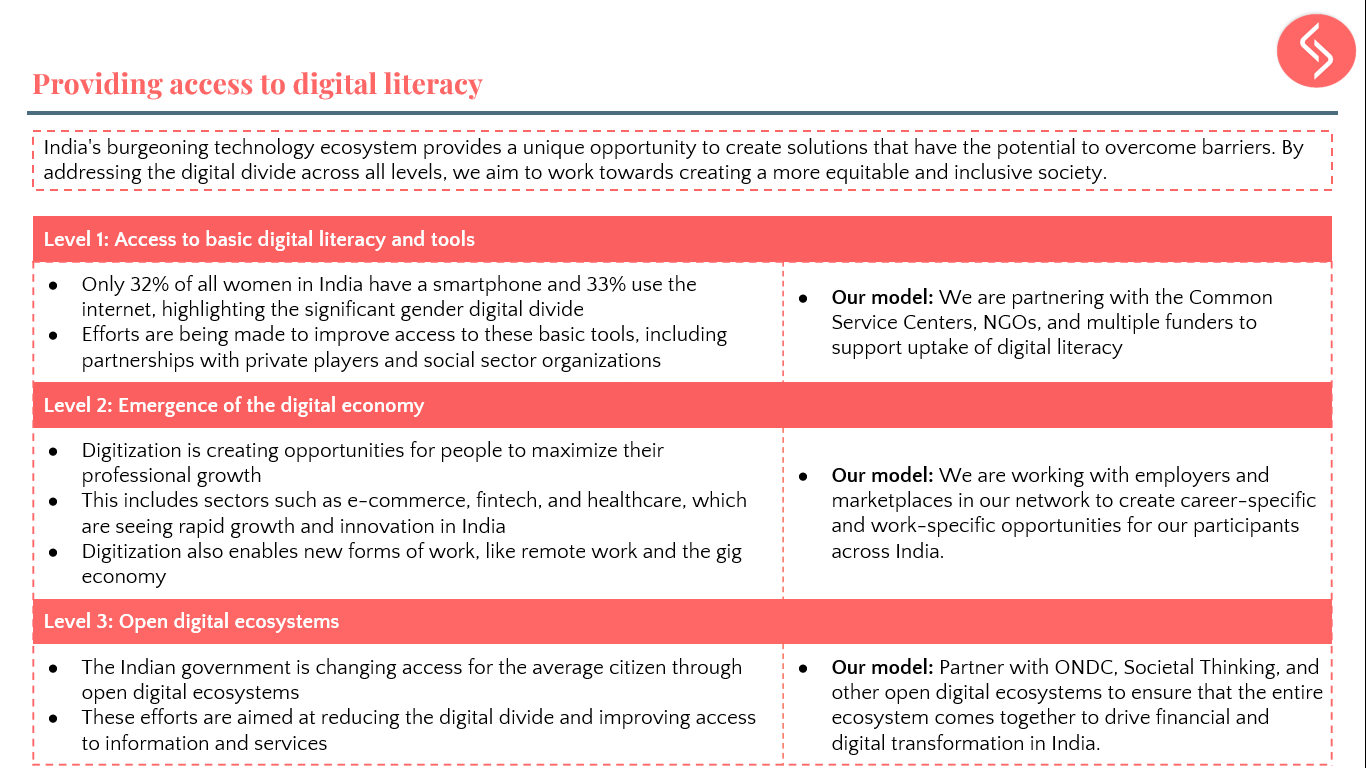
When women are empowered to make informed decisions about their reproductive health, they gain more control over their participation in the workforce, education, and income generation. To extend contraceptive awareness beyond the health sector, India must adopt a multi-sectoral approach. Collaboration between education, media, labor, and women’s empowerment sectors, alongside health, is essential to normalize conversations about family planning and expand access to comprehensive SRH education. Cross-sector partnerships, private sector engagement, and diversified funding are critical to making contraceptive awareness part of broader social, economic, and community efforts. In line with its mission to promote women’s holistic well-being, WOHLA focuses on creating demand for family planning while supporting social inclusion and women’s economic empowerment. WOHLA’s fourth partnership approach “layers” FP demand creation with services that enhance women’s livelihood opportunities. SRH/FP messaging is integrated into Common Service Centers, NGOs working on social inclusion, workplace initiatives, and skilling centers for beauty parlor entrepreneurs. These platforms serve dual purposes: they offer access to social protection schemes, digital and financial literacy, and credit, while also providing trusted spaces for women to discreetly inquire about SRH/FP products and services. This innovative model, led by the Collective Good Foundation (CGF)/Samhita in partnership with the Ministry of Electronics and Information Technology and their ecosystem of NGOs, ensures that SRH information is embedded in initiatives that promote women’s economic security and social inclusion.
5. Stewarding the health marketplace
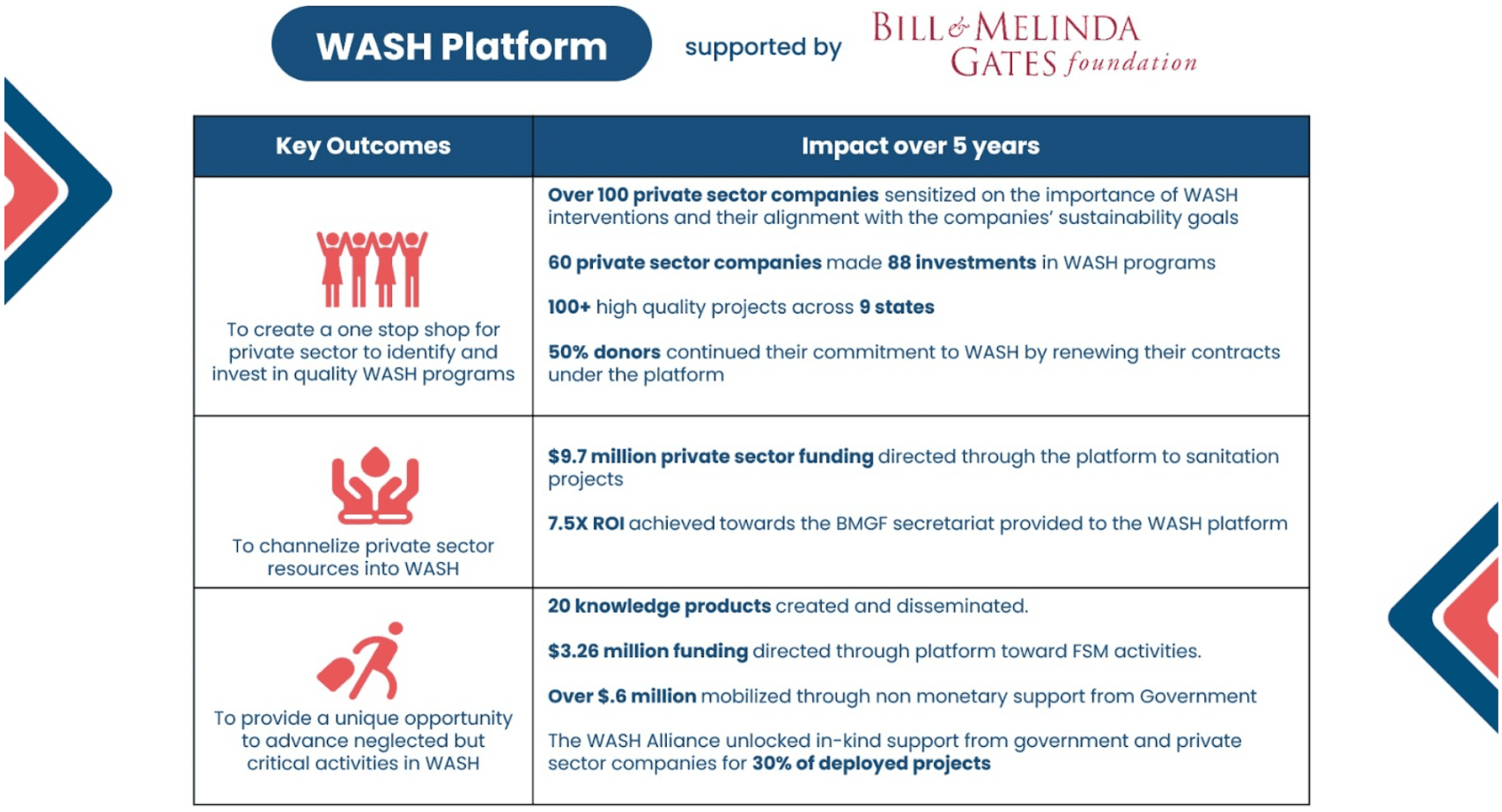
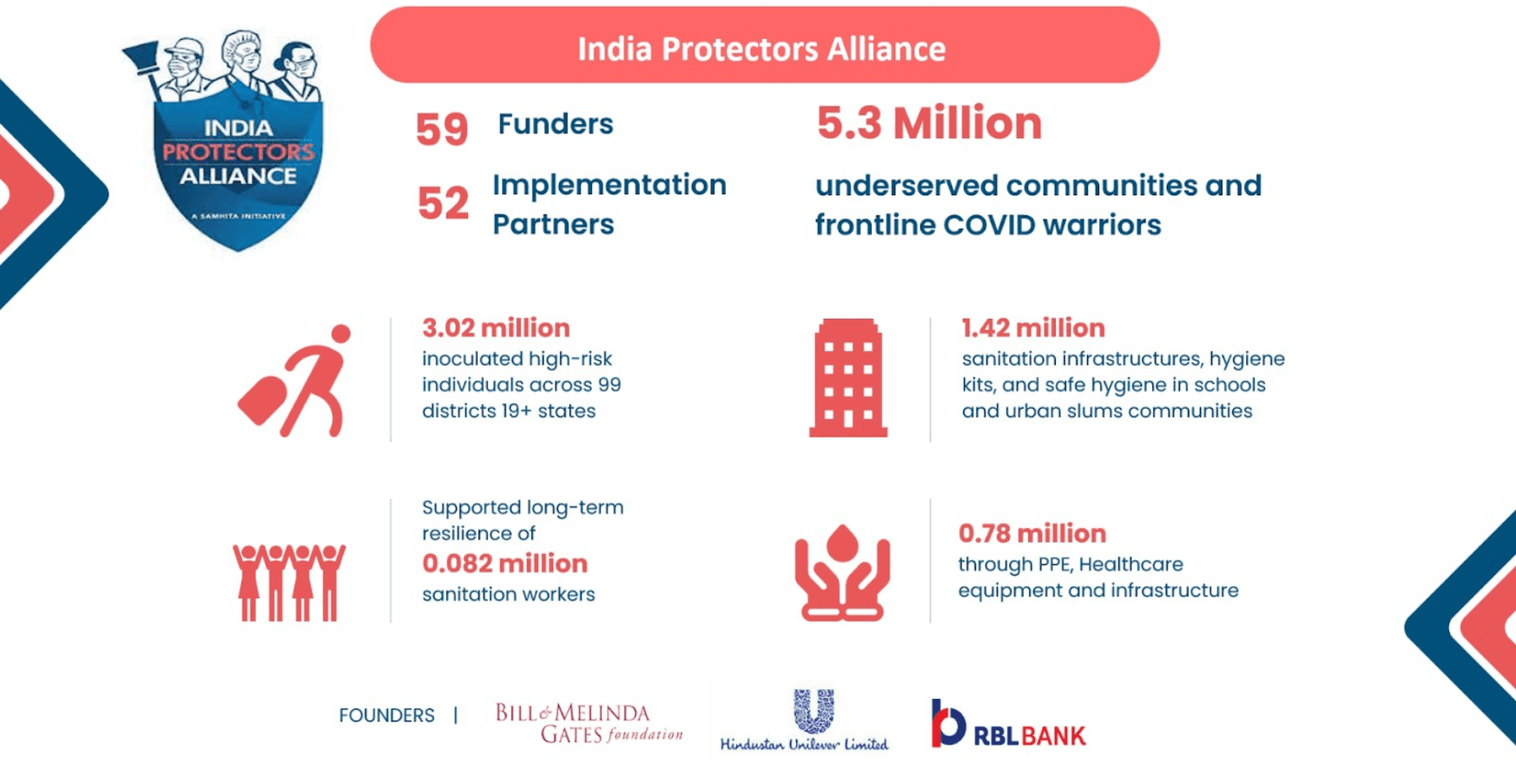
There is a lack of platforms or coalitions that coordinate entrepreneurs to align private sector actors and advocate for policies that improve access to women’s health services, especially for younger populations. Additionally, broader inter-ministerial and inter-sectoral engagement platforms are missing, which are essential for innovating strategies around contraceptive awareness and for leveraging corporate mandates focused on women’s economic empowerment and leadership. Hormonal contraceptives, which play a crucial role beyond pregnancy prevention by managing conditions like heavy menstrual bleeding, endometriosis, and uterine fibroids, are key to these discussions. Increasing awareness of these medical benefits requires a coordinated effort across sectors. By integrating hormonal contraceptives into broader health and empowerment initiatives through CSCs, private healthcare providers, and NGOs, we can normalize their use and reduce stigma, improving overall women’s health. WOHLA’s fifth partnership approach focuses on creating an integrative platform that fosters cross-sectoral collaboration. By uniting government, private sector actors, and NGOs, WOHLA aims to develop solutions for improving access to family planning (FP) and advancing women’s economic empowerment. Through the CGF/Samhita marketplace, WOHLA connects FP solutions with financing resources, driving greater private sector participation and expanding access to essential FP products like hormonal contraceptives.
6. Engaging the public sector for a supportive policy environment
India’s Vision FP 2030 highlights the critical need to enhance private sector engagement in family planning (FP). Despite efforts to involve the private sector, significant opportunities remain untapped. With government capacity stretched and FP resources dwindling, it’s essential to support government functionaries and program managers in bolstering private sector participation to ensure quality, accessibility, and sustainability of FP services nationwide. Challenges such as data sharing between public and private providers, and maintaining continuity of care, complicate the integration of private sector services into public health systems. Without effective stewardship and cross-sector collaboration, access to contraceptive products and services, especially in underserved regions, remains limited, hindering FP program success. Under this technical assistance through local partner, Access Health, the aim is to create an inclusive, competitive market for contraceptive options by 2030, focusing on regulatory engagement and harmonization efforts to address barriers like drug scheduling. This would ensure that newer contraceptives are available over the counter and included in national guidelines. A key strategy is integrating private AYUSH Medical Officers into the FP service framework, particularly in underserved areas. Future work emphasizes advocating for the inclusion of FP services in public and private insurance schemes, thereby expanding access and strengthening the overall provider base.
WOHLA is pioneering an ecosystem approach to shape a dynamic and sustainable family planning (FP) marketplace in India. Moving beyond traditional, narrow-focused contraceptive awareness initiatives, WOHLA’s comprehensive strategy brings together a diverse range of value chain actors—manufacturers, distributors, service providers, NGOs, private sector entities, and the government. By engaging these stakeholders across both supply and demand-side challenges, WOHLA aims to create a more integrated and efficient FP ecosystem.
The focus is on fostering collaboration to address bottlenecks in access, availability, and awareness of contraceptive options, ensuring a holistic approach to improving women’s health and economic well-being. This multi-stakeholder commitment is essential to advancing FP outcomes, which in turn, can lead to broader positive impacts for communities and the nation. Through this ecosystem approach, WOHLA seeks to build a marketplace where innovation, accessibility, and sustainability thrive, ensuring that contraceptive products and services are available to all women, particularly in underserved regions. By aligning the interests of all value chain actors, WOHLA is setting the stage for long-term, scalable improvements in reproductive health, empowering women and contributing to the country’s overall development.